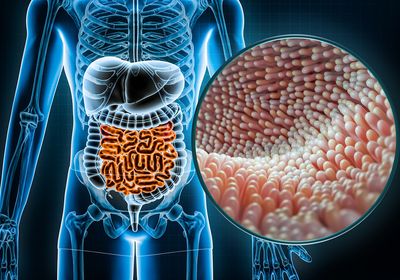
ABOVE: © iStock.com, selvanegra
Chimeric antigen receptor T cells, better known as CAR T cells, are powerful immunotherapy agents derived from a cancer patient’s existing immune cells and engineered to fight their specific tumors. However, as successful as they are in treating some cancers, they fail at treating others, such as pancreatic tumors, which develop clever ways of avoiding immune detection.
But such failures may soon be a thing of the past: In two new mouse studies published in Science on December 15, researchers unveiled tactics for creating manipulatable CAR T cells. The researchers behind the works say that, thanks to the new approaches, they may be able to overcome the current hurdles facing CAR T therapies. The new techniques allow them to control when and where CAR T cells are active, targeting tumors at specific times and keep CAR T cells from becoming less effective over time, which often happens during cancer.
Grégoire Altan-Bonnet, a systems immunologist at the National Institutes of Health (NIH) who coauthored a perspective on both studies in Science but was not involved in either, notes that doctors currently inject T cells into patients with the hopes that patients will respond to the treatment. With these new techniques, scientists will be able to activate and shut off CAR T cells, and “have them do what we want,” he says.
“We’re really seeing an acceleration of what can be done,” he adds. “We’re building a new immune response.”
Controlling where: Engineering a one-stop shop for targeting tumors
Chimeric antigen receptors (CARs) are synthetic proteins modeled on normal T cell receptors but are designed to home in on tumors. CARs are engineered into a patient’s own T cells, thereby providing the patient’s immune system with an army of cells ready to go after any cancerous cells they find. But this army struggles to tackle solid cancers, says Wendell Lim, a University of California, San Francisco cell and molecular biologist and a coauthor of one of the studies, because the environment around the tumor is immunosuppressive and blocks CARs, keeping the engineered cells from spotting their target.
One way to overcome this issue is to ramp up a patient’s immune system across the board to compensate for the suppression around the tumor. But since the tumors grow over the span of weeks or longer, such immune boosts need to last just as long—and prolonged immune activity can cause T cells to enter an “exhausted” state, in which they’re unable to kill cancer cells effectively. So Lim set out to solve the problem of immune suppression around the tumor.
We’re really seeing an acceleration of what can be done. We’re building a new immune response.”
—Grégoire Altan-Bonnet, National Institutes of Health
He and his lab first engineered CAR T cells to produce IL-2, an immune-boosting cytokine known to stimulate T cell growth. Lim says that IL-2 makes T cells more effective at infiltrating solid tumors and recruiting other T cells to join the attack, but when given systemically at high doses, the cytokine can have dangerous side effects, making localized delivery essential.
Unfortunately, getting IL-2 to where it’s needed and nowhere else is a tricky task. CAR T cells are activated when their CARs bind with tumor antigens, so in theory, engineering these cells to produce IL-2 when activated would lead to tumor-specific release of the cytokine. But that doesn’t work if the CARs are being blocked, so Lim and colleagues gave the cells an alternate activating receptor called synNotch, which they predicted would be able to bypass a tumor’s immunosuppressive tactics.
In human cells in vitro, synNotch was able to bind to a tumor’s antigens, activating and driving the dual-receptor-wielding CAR T cells to release IL-2. The IL-2 release caused engineered CAR T cells and cocultured, nonengineered T cells to multiply and ready themselves to fight the tumor. In a follow-up experiment, the researchers injected the re-engineered synNotch-containing CAR T cells into mice with pancreatic tumors and melanoma. Within 60 days after the injection, the T cells shrank or eliminated the tumors.
“What we found here is that when we did this, we could make cells that could kill very, very challenging cancers, like pancreatic cancer,” says Lim, adding that he’s excited by the results because they show “that it is possible to remodel a suppressive tumor environment.”
“What they’ve done is make a more intelligent CAR T cell,” says Michael Z. Lin, a bioengineer at Stanford who was not involved in either study, who describes Lim’s paper as “great.”
Controlling when: Remotely operating T cells using crafted gene circuits
While Lim and his team gave CAR T cells the power of self-activation, immunologist Ahmad Khalil’s lab at Boston University found another way to get CAR T cells to make IL-2 on demand, which they described in the other Science study published yesterday.
The team had set their sights on using existing cancer drugs to turn on certain CAR T cell genes, he explains. That way, they could activate specific genes at specific times and regulate the cells’ activity. They accomplished this by crafting synthetic transcription factors based on small, sandwich-shaped amino acid sequences called zinc fingers, which bind to DNA. Each of these synZFTRs, as they dubbed their new proteins, was designed to only bind to its target sequence in the presence of an established pharmaceutical. In that way, “we built these ‘gene switches’ that can be activated by or activated and regulated by these FDA-approved drugs,” explains Khalil.
The team then used their switches to attempt to control CAR expression in T cells. And it worked: They were able to induce CAR expression in response to the cancer drug tamoxifen, switching CAR T cells from an “off” state to a tumor-targeting “on” state.
In another experiment, they used a separate synZFTR involving a different drug to induce IL-2 release in T cells lacking CAR receptors. This made it so the scientists could trigger IL-2–driven proliferation both in vitro and in mice. “This ‘on demand’ kind of stimulation [of] proliferation could be a way . . . to get T cells fired up again” after they become exhausted, Khalil says.
I think the hope is that it captures the imagination of researchers and gets us thinking how we can engineer our cells to be more sophisticated and smarter.
—Ahmad Khalil, Boston University
Finally, they tested whether they could control both switches simultaneously or at different times inside the same animal. In theory, says Khalil, this could allow researchers to remote-control T cells to perform specific functions at a given time. “T cells take on different [functions] depending on the combination and the timing of the signals they receive,” says Khalil. “So we asked, ‘Can we synthetically mimic this?’ And the short answer is yes.”
By delivering two drugs to turn on different gene switches, the researchers found they could instruct T cells to produce CAR and then IL-2 at different time points. In a mouse model of pancreatic cancer, the researchers saw that inducing this sequential activation (first CAR, then IL-2) was more effective at clearing tumors than either treatment alone or simultaneous treatment.
Khalil says that this sort of transcriptional control could allow researchers to program cell types and control their activity, though that “is a little bit far out,” he admits. “But I think the hope is that it captures the imagination of researchers and gets us thinking how we can engineer our cells to be more sophisticated and smarter.”
Smarter T cells for treating challenging cancers
Though developed independently, Lim and Khalil’s approaches could be combined to create fine-tuned immunotherapies, Altan-Bonnet says. In tandem, the two approaches could be used to engineer CAR T cells that only activate when necessary.
The Lim lab’s technology could direct T cells to tumors, where they would receive the signal to attack. Then, with the technology from Khalil’s study, researchers could precisely control what that attack looks like and even shut the cells off, preventing them from reaching the point of exhaustion, suggests Altan-Bonnet. In that way, “researchers could arm T cells with multiple tools they need to take on tumors,” says Altan-Bonnet, and eliminate the need for systemic administration of therapies like IL-2 that can have nasty side effects.
Both Lim and Khalil say they hope to take their findings to the clinic in the future.