Targeted anti-cancer therapies dramatically improve patient outcomes in EGFR-mutant lung adenocarcinomas,1 but many tumors acquire resistance to these drugs over time. Because there are numerous ways in which cancers become resistant to therapies, scientists often do not know why particular tumors stop responding or how to re-sensitize them.
“This is a big unmet need in the field because in order to really get to the next step in the treatment of the disease, we need to understand these mechanisms of resistance,” said Katerina Politi, a cancer biologist at the Yale School of Medicine.
Politi and Cigall Kadoch, a cancer biologist at the Dana-Farber Cancer Institute and Harvard Medical School, recently published a paper in Cancer Cell addressing this question.2 Their research teams, led by co-first authors Fernando de Miguel and Claudia Gentile, wanted to understand the resistance mechanisms to the targeted tyrosine kinase inhibitor (TKI) osimertinib, which treats EGFR-mutant tumors. Osimertinib is a first-line therapy for this type of cancer, and resistance almost always develops.3
To explore this resistance, the researchers used five different EGFR-mutant lung cancer cell lines, all of which were sensitive to TKIs. To generate osimertinib-resistant versions of these cell lines, they exposed each to the drug, selected those that survived the treatment, and analyzed their exomes.
Politi and her team tried to find additional mutations in the EGFR gene responsible for the osimertinib resistance and came up empty-handed. As a result, the researchers postulated that an epigenetic mechanism that affected whether or not particular genes could be transcribed may be the culprit. They performed RNA sequencing to look at differences in gene expression between resistant and sensitive lung cancer cells and found many differentially up- and down-regulated genes.
Next, the researchers performed Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq), which looks at chromatin accessibility. They found that resistant cells had differentially-accessible genomic regions, and that more than 50 percent of gene expression changes corresponded with DNA accessibility changes at or near gene promoters or enhancers. When they examined these gene targets, the researchers found various genes and pathways modulated in the resistant state, such as upregulation of the EMT and RTK signaling pathways and downregulation of epithelial cell differentiation and cell-cell adhesion. These changes could lead to resistance by altering the cell’s dependence on the original oncogene, changing signaling, or modulating apoptosis. The researchers concluded that chromatin accessibility changes for key gene regulatory programs underlie the difference between parental and TKI-resistant EGFR-mutant cancer cell lines, and that epigenetic factors are likely to be playing a key role in resistance.
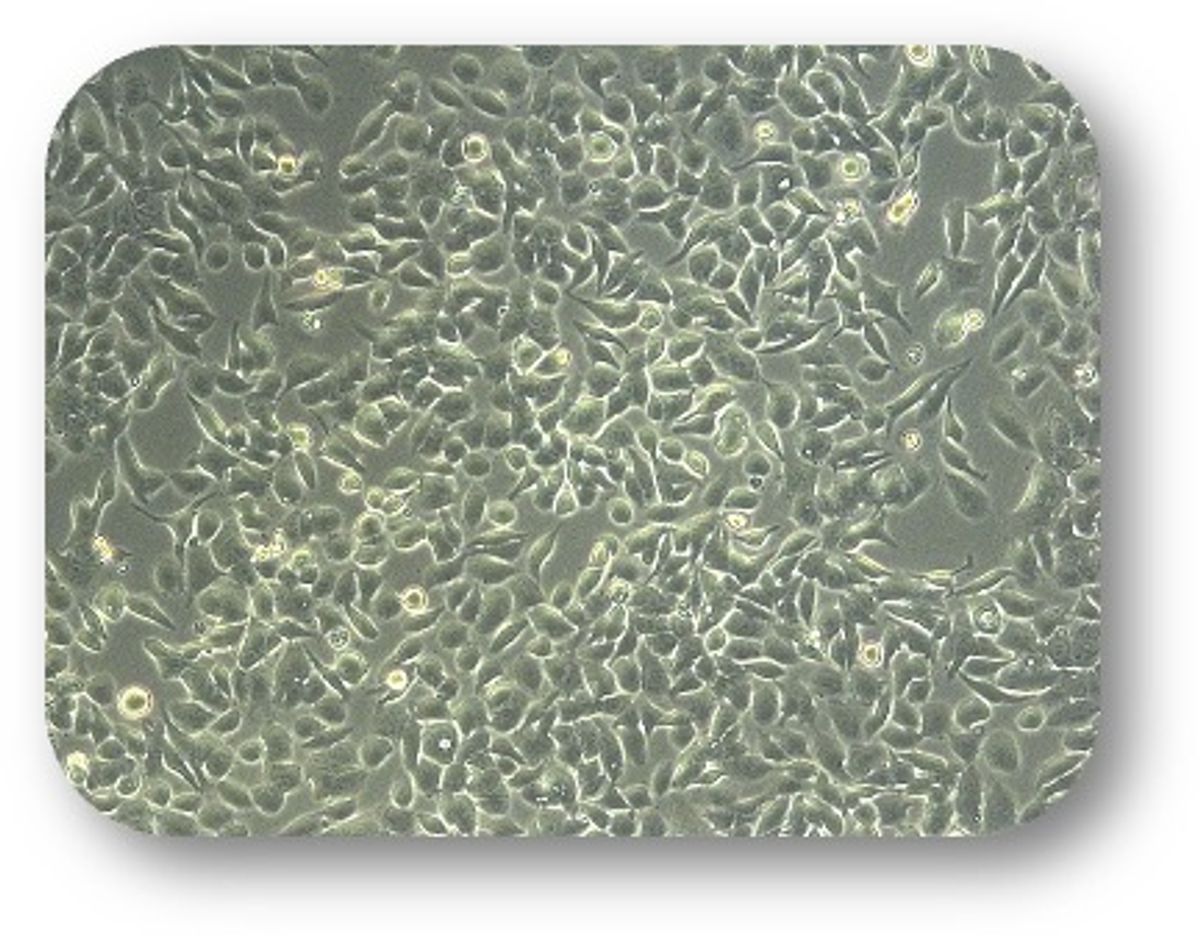
During these experiments, the researchers became particularly interested in the SMARCA4 protein, a key component of the chromatin remodeling complex mSWI/SNF. Using epigenome analysis, the researchers found that mSWI/SNF complexes were located at different sites across the genome in TKI-resistant lung cancer cell lines versus drug-sensitive cell lines. The presence or absence of mSWI/SNF altered chromatin accessibility and changed certain transcriptional programs.
To see if the cells could become re-sensitized to osimertinib, Politi, Kadoch, and their teams used short hairpin RNA to knock down SMARCA4 in the resistant cell lines. They also knocked out the gene in human EGFR-mutant, TKI-resistant tumors that had been implanted in mice. In yet another experiment, they used a drug to pharmacologically suppress SMARCA4’s activity in resistant cell lines. The researchers found that a subset of these resistant cancer models were re-sensitized to osimertinib.
“We think that the shift in chromatin accessibility that SMARCA4 and mSWI/SNF mediates in the resistant setting allows the cells to survive better, to proliferate and divide better, and also withstand the stresses that are imposed by drugs, by activating an antioxidant response in the cells,” said Politi. SMARCA4 knock-down in the presence of osimertinib elevated the levels of reactive oxygen species, which would help lead to their demise.
See also “Epigenetic Marks May Cause Brain Tumor Formation”
Finally, in mice harboring osimertinib-resistant, patient-derived xenografts of EGFR-mutant lung cancer, the researchers inhibited mSWI/SNF ATPase activity with a drug called FHD-286. When combined with osimertinib, this treatment slowed tumor growth. FHD-286 is currently in clinical development as a cancer therapeutic by Foghorn Therapeutics, co-founded by Kadoch.
“The pharmaceutical industry is very interested in targeting [SMARCA4],” said Mark Rubin, a prostate cancer researcher at the University of Bern who was not involved in this study. However, such drugs are often toxic because they affect both tumor and healthy cells. “This study provides a rationale for further developing these drugs to sensitize resistant cells. Epigenetic therapies are very important, and the challenge is how to bring them into the clinic,” said Rubin.
References
- Howlader N, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med. 2020; 383(7):640-9.
- de Miguel FJ, et al. Mammalian SWI/SNF chromatin remodeling complexes promote tyrosine kinase inhibitor resistance in EGFR-mutant lung cancer. Cancer Cell. 2023;41:1516-1534.
- Ramalingam SS, et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med. 2020; 382:41-50.