Stay up to date on the latest science with Brush Up Summaries. This Brush Up is sponsored by ATCC.
What Is Programmed Cell Death?
Programmed cell death (PCD) is a set of mechanisms that multicellular organisms use to self-destruct cells.1 This process is crucial during embryonic and post-embryonic development and for tissue maintenance.2 For example, during embryonic development PCD sculpts fingers and toes by removing the interdigital webs.2 PCD also occurs during stringent selection of B and T lymphocytes. This removes immune cells that target other cells in the body, preventing autoimmunity.3
Over the years, researchers have described many forms of PCD.4 This summary provides a brief overview of three types—apoptosis, pyroptosis, and necroptosis–and their importance in health and disease.1
Lytic Versus Non-lytic PCD
In general, PCD can be either lytic or non-lytic. During lytic cell death, the contents of a dying cell are released into the surrounding space as the cell’s membrane becomes damaged.4 In contrast, non-lytic cell death secludes the cellular remains in multiple apoptotic bodies before they are discarded.4
What Is Apoptosis?
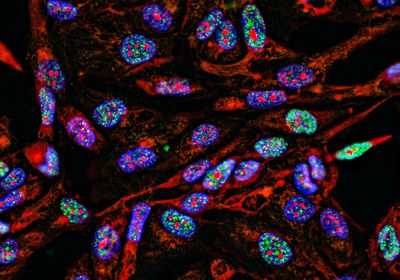
Apoptosis is a form of non-lytic PCD that involves condensation of the nucleus and cytoplasm, chromosomal cleavage, and plasma membrane blebbing.5 It was the first type of PCD to be described by scientists.5 There are two major mechanisms for apoptosis: intrinsic apoptosis and extrinsic apoptosis.
Intrinsic Versus Extrinsic Apoptosis
Intrinsic apoptosis occurs when a cell is damaged on the inside or is facing a stressful internal condition, such as DNA damage or nutrient deprivation. These conditions cause the mitochondrial outer membrane to permeabilize and release cytochrome C.1 Cytochrome C helps apoptotic protease-activating factor 1 (APAF-1) proteins assemble into a larger unit in the cytoplasm. APAF-1 is key during apoptosis because it contains a caspase recruitment domain (CARD), which activates protease enzymes called caspases that cleave proteins.1
Unlike intrinsic apoptosis, extrinsic apoptosis is triggered by a signal outside of the cell and requires membrane-spanning proteins called death receptors.6 The external signal, or death ligand, can come from another cell or environmental response. Activation of death receptors by death ligands such as Fas, tumor necrosis factor (TNF), or TNF-related apoptosis-inducing ligand (TRAIL), recruits two proteins to form a death-inducing signaling complex (DISC), which activates a different set of caspases from intrinsic apoptosis.6
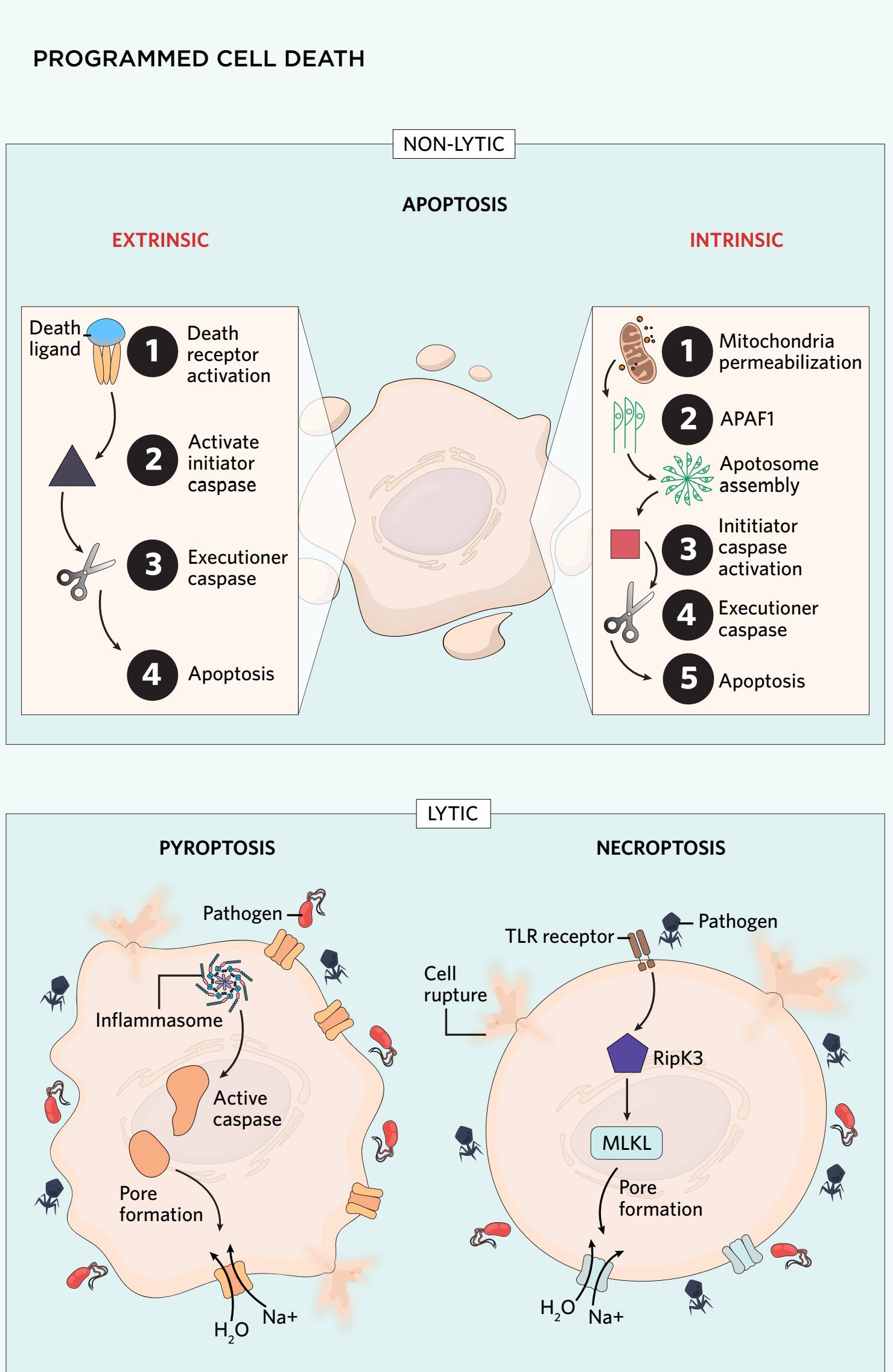
In both extrinsic and intrinsic apoptosis, the first caspases activated by either APAF-1 or DISC are called initiator caspases. Initiator caspases activate executioner caspases to carry out mass protein breakdown throughout the cell. In extrinsic and intrinsic apoptosis, this destruction induces the formation of apoptotic bodies through blebbing of the plasma membrane into smaller vesicles. These vesicles contain the dying cell’s contents, which are later engulfed by phagocytic cells.7
What Are Necroptosis and Pyroptosis?
Necroptosis and pyroptosis are categorized as regulated necrosis and are lytic forms of PCD.1 When cells experience traumatic injury, the trauma often causes unregulated necrosis, where cells swell and rupture uncontrollably from increased pressure.8 In contrast, cells can self-destruct in a controlled, regulated fashion via necroptosis and pyroptosis by forming pores in the membrane to facilitate cell rupturing due to increased water and ion influx.8
Pyroptosis Mechanism
Pyroptosis most often occurs when a cell is infected with an intracellular pathogen.9 Parts of the pathogens called pathogen-associated molecular patterns (PAMPs) cause an inflammasome complex to form. The inflammasome activates different caspases than those in apoptotic PCD, which assist with membrane pore formation.9 Pore formation releases damaged-associated molecular patterns (DAMPs) and cytokines into the extracellular space, eliciting an immune response to recruit immune cells to remove the damaged or infected area.9
Necroptosis Mechanism
Necroptosis is also initiated by pathogen infection. However, instead of forming the inflammasome, necroptosis requires the formation of a protein complex called the necrosome.10 The necrosome contains the mixed lineage kinase domain-like (MLKL) protein, which is phosphorylated by a receptor-interacting serine/threonine-protein kinase 3 (RIPK3), inducing a conformational change in MLKL.10 This conformational change enables MLKL to translocate to the plasma membrane and form pores. Necroptosis does not require caspase activation to compromise the integrity of the plasma membrane. In fact, caspase-8 must be blocked to enable phosphorylation of the RIPK proteins.10 Like pyroptosis, cellular contents including DAMPs leak through the pores and elicit an immune response.
Role of Autophagy in Programmed Cell Death
Autophagy is often used by cells as a survival mechanism to protect itself from nutrient deprivation, oxidative stress, endoplasmic reticulum stress, etc.11 Here, the cytoplasm is sequestered and packaged for degradation by the lysosome, rather than being release into the extracellular space. In many cases, the material that is degraded by the lysosome can be recycled and used again as starting materials, such as amino acids for protein synthesis or carbohydrates for energy production.12 Before the material is degraded by the lysosome, it is packaged into a double-membrane autophagosome. This form of autophagy is known as macroautophagy, but other types of autophagy exist, including microautophagy and chaperone-mediated autophagy. The latter examples do not involve formation of an autophagosome, and the contents to be degraded are either directly taken up by the lysosome or are chaperoned across the lysosomal membrane.12 Although researchers have previously characterize autophagy as a form of cell death, due to dying cells often containing autophagic vacuoles, this characterization is often viewed as paradoxical because in most circumstances autophagy promotes cellular survival.13
Programmed Cell Death Dysregulation in Disease
PCD in Neurodegenerative Diseases
PCD dysregulation can be dangerous for disease progression and initiation. In the case where there is more PCD than normal, the body is not able to recuperate the increased cell death. An example of this is in neurodegenerative diseases such as Parkinson’s disease, Huntington’s disease, and amyotrophic lateral sclerosis (ALS).14
In ALS, there is aberrant motor neuron death in the spinal cord and cerebral cortex, leading to muscle weakness. Over 20 percent of patients with ALS have a mutation in a protein called superoxide dismutase 1 (SOD1).14 This mutation causes SOD1 to bind and block an anti-apoptotic protein, B cell lymphoma-2 (BCL-2), in spinal cord neurons, which promotes aberrant apoptosis.
In Parkinson’s disease, mutant Parkin enzyme no longer ubiquitinates BCL-2 antagonistic killer 1 (BAK), a protein which promotes mitochondrial permeabilization. This causes apoptosis of dopaminergic neurons in the brain.14
PCD and cancer
In contrast to diseases with enhanced apoptosis, cancer cells have mechanisms in place that help them evade PCD. By avoiding PCD, they can persist in the body and continue proliferating. For example, many hematological and solid tumor cancers have increased expression of the anti-apoptotic BCL-2 protein, which sequesters pro-apoptotic proteins to inhibit PCD.15
Researchers are developing cancer therapy drugs to target proteins involved in PCD evasion. For example, the BCL-2 inhibitor venetoclax selectively binds BCL-2 and displaces its sequestered pro-apoptotic proteins.16 Researchers are testing this drug in nearly 200 clinical trials to understand its efficacy in the treatment of leukemias, such as acute myeloid leukemia and chronic lymphocytic leukemia.15,16
References
- N. Ketelut-Carneiro, K.A. Fitzgerald, "Apoptosis, pyroptosis, and necroptosis—oh my! the many ways a cell can die," J Mol Bio, 434(4):167378, 2022.
2. Y. Fuchs , H. Steller, "Programmed cell death in animal development and disease," Cell, 147(4):742-58, 2011.
3. J.T. Opferman, S.J. Korsmeyer, "Apoptosis in the development and maintenance of the immune system," Nat Immunol, 4(5):410-15, 2003.
4. L. Bedient et al., "Lytic cell death mechanisms in human respiratory syncytial virus-infected macrophages: roles of pyroptosis and necroptosis," Viruses, 12(9):932, 2020.
5. A. Ashkenazi et al., "From basic apoptosis discoveries to advanced selective BCL-2 family inhibitors," Nat Rev Drug Discov, 16(4):273-84, 2017.
6. P. Nair et al., "Chapter Five - Apoptosis initiation through the cell-extrinsic pathway, in Methods in Enzymology, eds. A. Ashkenazi, J. Yuan, J.A. Wells, Vol. 544, Academic Press, 2014. pp. 99-128. (Regulated Cell Death Part A: Apoptotic Mechanisms).
7. G. Wickman et al., "How apoptotic cells aid in the removal of their own cold dead bodies," Cell Death Differ, 19(5):735-42, 2012.
8. T.V. Berghe et al., "Regulated necrosis: The expanding network of non-apoptotic cell death pathways." Nat Rev Mol Cell Biol, 15(2):135-47, 2014.
9. T. Bergsbaken et al., "Pyroptosis: Host cell death and inflammation," Nat Rev Microbiol, 7(2):99-109, 2009.
10. J. Seo et al., "Necroptosis molecular mechanisms: Recent findings regarding novel necroptosis regulators," Exp Mol Med, 53(6):1007-17, 2021.
11. O. Kapuy et al., "Autophagy-dependent survival is controlled with a unique regulatory network upon various cellular stress events," Cell Death Dis, 12(4):1-11, 2021.
12. K.R. Parzych, D.J. Klionsky, "An overview of autophagy: Morphology, mechanism, and regulation," Antioxid Redox Signal, 20(3):460-73, 2014.
13. S Jung et al., "Autophagy as a decisive process for cell death," Exp Mol Med, 52(6):921-30, 2020.
14. D. Moujalled et al., "Molecular mechanisms of cell death in neurological diseases," Cell Death Differ, 28(7):2029-44, 2021.
15. A. Strasser, D.L. Vaux, "Cell death in the origin and treatment of cancer," Mol Cell, 78(6):1045-54, 2020.
16. A. Sharma et al., "Cancer metabolism and the evasion of apoptotic cell death," Cancers, 11(8):1144, 2019.