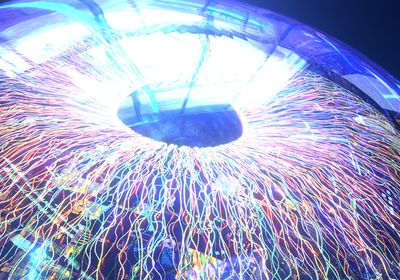
ABOVE: The cornea is a transparent layer of tissue that protects the eye from infection. New research shows that the cornea is inhabited by adaptive immune cells, like T cells, not only innate immune cells like dendritic cells as previously believed. © iStock, aislan13
The cornea is akin to a battlefield. Constantly exposed to pathogens, it plays a critical role in protecting the eye from diseases.1 Yet for years, ocular immunologists agreed that the human cornea was only inhabited by innate immune cells like dendritic cells (DCs).2
In a paper published in Proceedings of the National Academy of Sciences, optometrist Holly Chinnery and her colleagues at the University of Melbourne challenged this consensus by reporting the presence of specialized T cells—a type of adaptive immune cells—in the cornea.3 “It really questions some of our fundamental assumptions around the immune cells in the cornea, and that might challenge our thinking more broadly about diseases and therapies as well,” said Chinnery.
The consensus about innate immune cells in the cornea was based on in vivo confocal microscopy (IVCM), the current gold standard static imaging technique.3 However, IVCM has a few limitations, according to Chinnery. To better understand the cornea and its immune cells, Chinnery and her coauthor Laura Downie pioneered a new technique for dynamic corneal imaging: functional in vivo confocal microscopy (Fun-IVCM).
“We can capture the same area of the corneal tissue over time, and we take repeated images over a few minutes in between each image, and then can piece those together to form a time lapse video,” explained Downie.
Unlike traditional IVCM, Fun-IVCM can also capture images at different depths of the tissue. Leveraging this functionality of Fun-IVCM, Downie and Chinnery saw the immune cells moving around through the layers of the cornea, as if patrolling the tissue. This was an unexpected result, since they assumed the cells in question were DCs, which don’t behave that way.
See also “Science Snapshot: Eye Immunity”
In their previous studies with immunologist Scott Mueller at the University of Melbourne, the team observed tissue-resident memory T cells (Trm cells) in the corneas of lab mice in response to infection.4
“That was the lightbulb moment for me,” said Mueller, who also coauthored the current paper. “This cell is moving around that looks exactly like a T cell in a mouse. That's when we went down the path of proving that they were actually T cells for this study.”
To do so, the authors performed Fun-IVCM on healthy human subjects and compared the morphology and behavior of the cells they videoed with those they found in mice. The movement and morphology of the cells was akin to the T cells seen in mouse corneas following viral infection.

Next, they performed Fun-IVCM on individuals before and after they were exposed to inflammatory stimuli, demonstrating the response of the corneal cell populations to the inflammation. Acute inflammatory stimuli in the form of contact lens application reduced the number of T cells in the cornea. Chronic inflammation in the form of untreated ocular allergy did not affect the number of T cells, but it enhanced their motility.
Jeremías Galletti, an ophthalmologist and ocular immunologist at the National Academy of Medicine of Buenos Aires who was not involved in the study, said that the findings are very convincing. “This is a great paper. We usually think of the cornea as an immune-privileged organ, and that the rules of immunology are different there. But now, [the authors] have found that in healthy human subjects, we have T cells entering and leaving the cornea all the time,” Galletti commented.
The authors emphasized that Fun-IVCM could transform the broader field of ocular immunology, allowing clinicians and researchers to monitor populations of Trm cells in the cornea over long periods of time. They suggested that with further research and development, Trm cell populations could potentially be used as biomarkers of broader immune cell dynamics or disease pathophysiology and could even be used to evaluate the efficacy of therapeutics.
Paul McMenamin, retired ocular immunologist and Chinnery’s former graduate school supervisor who was not involved in the study, said that the discovery is groundbreaking for the field. “It’s like the first time somebody's invented a drone that goes above the battlefield. All of a sudden, you're looking down on the battlefield, and you can see individual soldiers,” McMenamin remarked. “It changes everything.”
References
- Niederkorn JY. Cornea: Window to Ocular Immunology. Curr Immunol Rev.2011;7(3):328-335.
- Niederer RL, McGhee CNJ. Clinical in vivo confocal microscopy of the human cornea in health and disease. Prog Retin Eye Res. 2010;29(1):30-58.
- Downie LE, et al. Redefining the human corneal immune compartment using dynamic intravital imaging. Proc Natl Acad Sci. 2023;120(31):e2217795120.
- Loi JK, et al. Corneal tissue-resident memory T cells form a unique immune compartment at the ocular surface. Cell Rep. 2022;39(8).