The CRISPR-Cas9 system revolutionized the way researchers manipulate DNA and introduced a new era in gene editing therapy. In cancer research, CRISPR-based therapy represents an exciting therapeutic approach through the genetic inactivation or repair of cancer-related genes.1 However, CRISPR therapies for solid tumors still face considerable challenges. Because these cancer cells replicate easily, therapies need to access numerous cells to reverse malignancy.2 This challenge is exacerbated by the fibrous and physically dense tumor microenvironment, which blocks CRISPR machinery.3
Early in his career, Daniel Siegwart used materials engineering to solve biomedical problems. After moving to the University of Texas Southwestern Medical Center, Siegwart applied these skills to animal cancer models, experimenting with lipid-based nanoparticles (LNPs) for delivering therapeutic nucleic acids. “When the CRISPR papers came out, we immediately read those papers and kind of fell out of our chairs because we could see very clearly this elusive discovery of a modular engineering tool,” said Siegwart. “There was a feeling that CRISPR is this hot, exciting, new technology. But how do you use it in cancer therapy when the efficiency is 1 percent and what you really need to do is kill every cell that grows?”
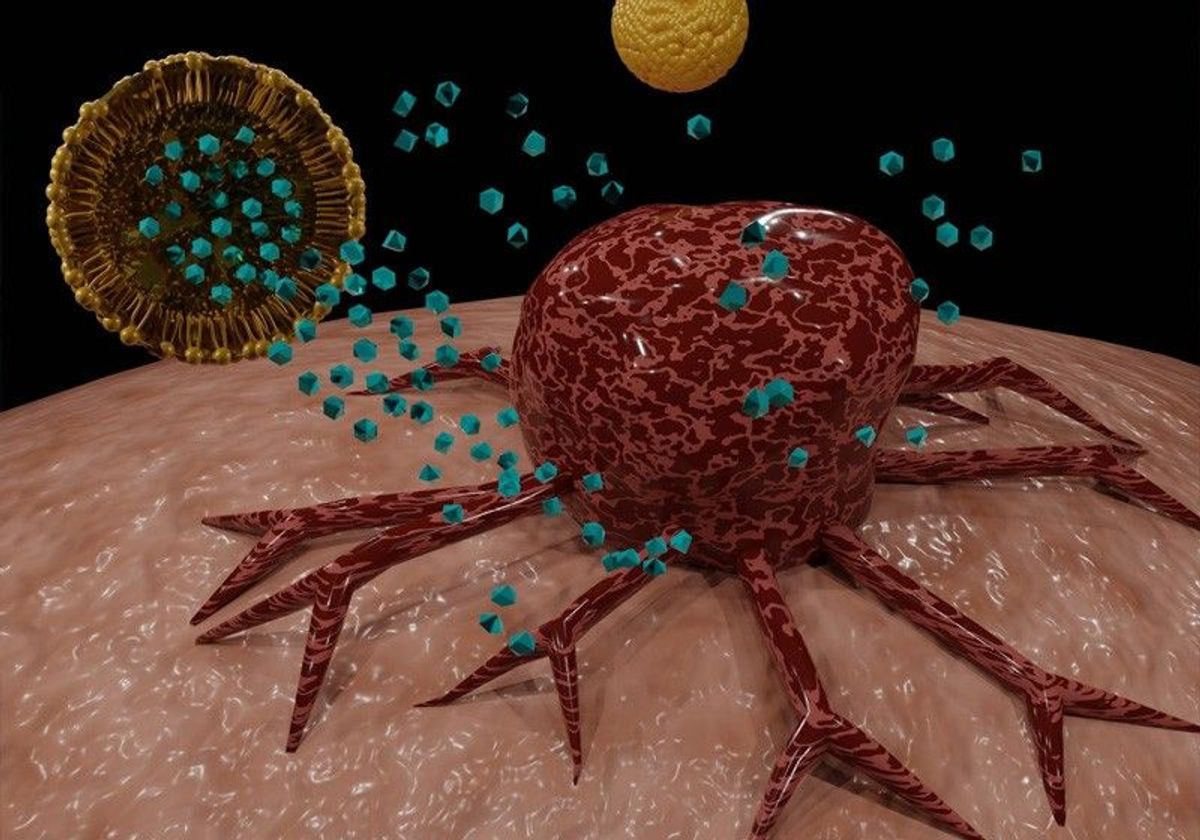
In a paper recently published in Nature Nanotechnology, Siegwart and his team developed a dual approach using LNPs equipped with tools that allow them to access and modify the tumor.4 The researchers packaged the LNPs with a CRISPR-Cas9 system that genetically modified and disrupted PD-L1 gene expression. PD-L1 overexpression inhibits T cell infiltration within the tumor microenvironment, so deactivating the gene allows immune cells to access the tumor. To grant the CRISPR system and immune cells tumor access, the LNP also included siRNA that targeted and reduced the expression of focal adhesion kinase (FAK), which diminished the density of the extracellular matrix surrounding the tumor.
There was a feeling that CRISPR is this hot, exciting, new technology. But how do you use it in cancer therapy when the efficiency is 1 percent and what you really need to do is kill every cell that grows?
- Daniel Siegwart, University of Texas Southwestern Medical Center
“To our surprise, we found that the [CRISPR] mRNA delivery efficacy was increased by FAK inhibition,” said Siegwart. The researchers found that this packaged nanoparticle delivery system enhanced gene editing by greater than 10-fold in tumor cell culture. When they tested the same therapy in mice, the results showed high levels of gene editing that overcame cancer cell replication, reduced tumor burden, and extended survival in four different cancer models, including solid ovarian and liver tumors. Overall, the novel LNP strategy revealed that reducing tumor tissue stiffness improved CRISPR gene editing in solid tumors.
“The degree of tumor control in the in vivo experiments was very good,” said Lukas Dow, a professor at Weill Cornell Medicine in New York who was not involved in the study. “Does that provide a window of opportunity in a clinical setting to capitalize on it? Would this be something that could allow [enough] tumor control to then follow up with other therapies?” asked Dow.
In future studies, Siegwart and his team are hoping to find more ways to use this new CRISPR delivery technology, including in conjunction with existing therapies. “This study…demonstrated the ability to combine multiple therapeutic agents in one nanoparticle. Therefore, we would like to use this strategy for other tumors that have similar measures to their matrix barriers and try other diseases that also have physical barriers, like fibrosis models,” Siegwart said.
References
- C.H. Huang et al., “Applications of CRISPR-Cas enzymes in cancer therapeutics and detection,” Trends Cancer, 4:499-512, 2018.
- D.B. Cox et al., “Therapeutic genome editing: Prospects and challenges,” Nat Med, 21:121-131, 2015.
- H. Jiang et al., “Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy,” Nat Med, 22:851-860, 2016.
- D. Zhang et al., “Enhancing CRISPR/Cas gene editing through modulating cellular mechanical properties for cancer therapy,” Nat Nanotechnol, 17:777-87, 2022.