Glioblastoma (GBM) is the most common and aggressive malignant tumor in the central nervous system, with a five-year survival rate as low as 6.8 percent.1 GBM tumors are heterogeneous, which poses major challenges for prognosis and treatment. Not only do these tumor cells have different expression profiles, but their cellular subtypes and spatial organization can also vary among patients, according to studies using single-cell RNA sequencing (scRNA-seq).2
While these previous experiments provided researchers with tumor cell transcriptome profiles, the tissue dissociation required for scRNA-seq sample preparations meant that they could not capture the spatial dynamics of cellular interactions. Retaining spatial information while assessing GBM prognosis is important because cellular interactions and tumor architecture play critical roles in driving clonal evolution, tumor progression, and therapeutic resistance.3-5 Therefore, researchers recently developed spatial transcriptomic profiling techniques in intact tissue to explore how cellular composition and spatial architecture contribute to GBM prognosis.6
One problem with this new approach is that scRNA-seq and spatial transcriptomics are expensive and have limited clinical applications as they are not routinely assayed as part of cancer diagnosis. However, there are inexpensive methods for GBM prognosis. For example, though staining tissue sections to obtain histology images does not provide transcriptome data or spatial information, this procedure is widely available and easier to obtain. In a recent Nature Communications paper, researchers combined these high- and low-tech methods to develop a GBM prognosis tool that predicts transcriptional subtypes from histology images.7
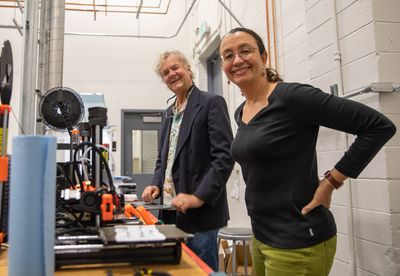
“We are very interested in bringing lots of different data modalities together,” said Olivier Gevaert, an expert on biomedical informatics from Stanford University and the senior author of the paper. “Especially linking, for example, imaging modalities with other types of modalities like molecular data.”
To build this tool, the Gevaert and his team first determined how cells with different transcriptome profiles were spatially organized. They analyzed three spatial transcriptomics datasets from 22 GBM patients to differentiate malignant spots from normal tissue. To determine different transcriptional subtypes, the researchers then analyzed transcriptomes from these malignant spots. In a complementary approach, they estimated the fractions of different cell types within each spot by using reference scRNA-seq datasets. Through these approaches, the researchers identified five distinct cell subtypes that could affect GBM patient prognosis. These cell populations included previously reported cellular states with neural progenitor, oligodendrocyte progenitor, astrocyte, and mesenchymal properties.8
To find out if these transcriptional subtypes could be predicted directly from histology images, the researchers developed a deep learning model. After training, evaluating, and validating this model, the Gevaert and his colleagues phenotyped over 40 million tissue spots from 920 whole-slide images across two independent cohorts and constructed high-resolution cellular maps in 410 GBM patients. Data analysis revealed that GBM prognosis differed significantly between transcriptional subtypes. Tumor cells expressing hypoxia-induced transcripts showed the worst prognosis. Moreover, the clustering of astrocyte-like cells led to a worse prognosis, while dispersion and connection of these cell types with other subtypes correlated with a better prognosis. Taken together, these data show that tumor cells’ response to a hypoxic environment and inflammation leads to a poor GBM prognosis.
To make their trained image models accessible for future research, the researchers developed GBM360, a user-friendly software that predicts and visualizes transcriptional subtypes and prognosis from histology images. “This is not approved for clinical use,” said Gevaert. “It's more of a demonstration…where people can upload their slides and then they can apply our model.”
“Their observations and conclusions could potentially be useful to create virtual histology biomarkers in the future,” Aydogan Ozcan, an expert on machine learning from the University of California, Los Angeles who was not involved in the study, said in an email. However, he pointed out that “how transferable these models are across different patient populations and malignancies would be important to evaluate at a larger scale.”
References:
- Ostrom QT, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol. 2019;21(Suppl 5):v1-v100.
- Tanay A, et al. Scaling single-cell genomics from phenomenology to mechanism. Nature. 2017 Jan 18;541(7637):331-338.
- Hara T, et al. Interactions between cancer cells and immune cells drive transitions to mesenchymal-like states in glioblastoma. Cancer Cell. 2021;39(6):779-792.e11.
- Venkataramani V, et al. Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature. 2019;573(7775):532-538.
- Osswald M, et al. Brain tumour cells interconnect to a functional and resistant network. Nature. 2015;528(7580):93-98.
- Ravi VM, et al. Spatially resolved multi-omics deciphers bidirectional tumor-host interdependence in glioblastoma. Cancer Cell. 2022;40(6):639-655.e13.
- Zheng Y, et al. Spatial cellular architecture predicts prognosis in glioblastoma. Nat Commun. 2023;14(1):4122.
- Neftel C, et al. An integrative model of cellular states, plasticity, and genetics for glioblastoma. Cell. 2019;178(4):835-849.e21.