ABOVE: Although the brain is rich in lipids, they are inaccessible to cancer cells. Researchers found that tumor cells that metastasized in the brain synthesized new fatty acids. © iStock, Jolygon
The monoclonal antibody Herceptin drastically improves prognosis for patients with HER2+ breast cancer. But if the primary tumor metastasizes to the brain, it often fails to respond to treatments.
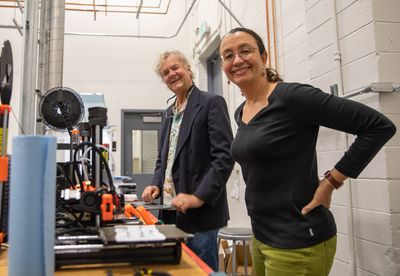
“Initially, this was thought to be the case because Herceptin is an antibody and it doesn’t cross the blood brain barrier. This led to the development of small molecule HER2 inhibitors, which do cross the blood brain barrier, but they also fail to control a lot of brain disease,” said Matthew Vander Heiden, Director of the Koch Institute for Integrative Cancer Research at MIT and senior author of a new study published in the journal Nature Cancer.1 “But increasingly, it’s been very clear that it’s not just the blood brain barrier, but something about growing in the brain. There are other microenvironmental differences.”
Beyond serving as a functional barrier to protect the brain from toxins, the blood brain barrier limits access to essential nutrients from peripheral circulation, necessitating metabolic adaptations for cancer cells to survive in this harsh environment. To begin to unpack the complex metabolic milieu of tumors, the researchers analyzed a published dataset with gene expression information on BT474 tumors, a human breast carcinoma with high HER2 expression.
Vander Heiden’s team observed a marked enrichment of genes involved in lipid metabolism in BT474 tumors that metastasized to the brain. To explore this, the researchers turned to a mouse model with human BT474 cells injected into either the mammary fat pad (MFP) or brain of immunodeficient mice. In these mice, they observed an increase in enzymes involved in fatty acid synthesis such as fatty acid synthase (FASN), in brain tumors compared to MFP tumors.
“From a 50,000-foot view, I’m thinking the brain has plenty of fat. It must be turning on lipids to solve some other problem,” said Vander Heiden.
When the team analyzed the extracellular fluid taken from healthy tissues, they found that the brain was lipid-poor compared to the MFP microenvironment. Although the brain does have lipids, they are often specialized lipids that are inaccessible to cancer cells.
“When we found there weren’t any there, that was kind of like a ‘duh, we should have thought of that’ moment,” Vander Heiden recalled. “That opened up the whole rest of the study.”
The researchers next used CRISPR-Cas9 to study FASN. Decreasing FASN impaired fatty acid synthesis and brain tumor growth, which improved mouse survival. Pharmacological inhibition of FASN increased cell death, but only when the researchers depleted lipids from the culture medium. From these studies, Vander Heiden’s team drew the conclusion that the dearth of lipids in the brain tumor microenvironment drives a dependency on de novo fatty acid synthesis.
“Understanding what helps brain metastases be different is really crucial to trying to target brain metastases, for which there are really very few therapies,” said Sheheryar Kabraji, an oncologist at the Dana Farber Cancer Institute and instructor at Harvard Medical School, who was not involved in the study.
While FASN inhibition shows promise for developing a therapeutic approach, Kabraji noted that targeting metabolic vulnerabilities is complicated; treating cancer will likely require orthogonal approaches.
“You can imagine a perfect therapeutic combination might be one that targets cancer signaling, alters cancer metabolism to make it pro-mutagenic, and then targets the immune environment. I think these are the kinds of therapies that we are hopefully moving towards,” said Kabraji.
Reference
- Ferraro GB, et al. Fatty acid synthesis is required for breast cancer brain metastasis. Nat Cancer. 2021;2:414-428.
This story was originally published on Drug Discovery News, the leading news magazine for scientists in pharma and biotech.