Cancer therapies have come a long way since researchers designed the first radiation and chemotherapy treatments.1 In the past, most cancer researchers focused on finding a single cure for cancer. However, scientists found that the molecular disease mechanisms were highly variable both in different cancers and among the same cancer types. Genetic heterogeneity between and within tumors is now established for most cancers, but this does not explain all tumor progression cases, and cancer remains one of the most prevalent diseases in the country.
The field of epigenetics is now at the forefront of cancer research. Epigenetic changes such as DNA methylation and acetylation alter cell functions without disrupting the DNA code. These changes are common in tumors, but researchers have not yet defined their role in cancer.2 In a recent paper in Cell, researchers at Harvard Medical School revealed that changes in epigenetic methylation patterns directly caused brain tumor formation in mice.3
People think of cancer as a genetic disease…caused by mutations, typically. But there's also a lot of evidence that in all cancers the methylation of the DNA is really deranged.
-Bradley Bernstein, Harvard Medical School
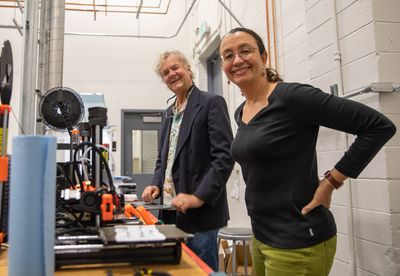
“People think of cancer as a genetic disease…caused by mutations, typically. But there's also a lot of evidence that in all cancers the methylation of the DNA is really deranged,” said Bradley Bernstein, a cancer biologist at Harvard Medical School and the senior author of the study. “The problem is, it's really hard to show whether that's driving the tumor or not.”
To better understand cancer formation, Bernstein and Gilbert Rahme, now a professor at Stony Brook University and first author of the paper, studied the resulting epigenetic changes from mutations in isocitrate dehydrogenase (IDH) that cause hypermethylation in certain human brain tumors. “The question we wanted to answer was whether any epigenetic changes that are observed in these specific kinds of brain tumors can actually drive a normal cell to make it cancerous,” said Rahme.
Bernstein had previously examined human tissue from IDH mutant gliomas and found that hypermethylation at an insulator site negatively regulated the expression of PDGFRA, an oncogene frequently upregulated in gliomas.4 In the current work, the researchers used CRISPR-Cas9 gene editing to disrupt this insulator region in mouse oligodendrocyte progenitor cells (OPCs)—a cell population which may give rise to gliomas. The mutation allowed an OPC-specific enhancer to activate PDGFRA gene expression, mirroring the effect of blocking the site with methylation in human cells. In addition to increased PDGFRA expression, the disruption increased OPC proliferation.
Next, the researchers explored if hypermethylation in IDH mutant gliomas affected any tumor suppressors. The researchers found evidence of CDKN2A downregulation along with methylation at this tumor suppressor’s promoter in clinical samples. As a result, they hypermethylated this region in OPCs in vitro, which silenced the gene and increased OPC proliferation. After, Bernstein and his team disrupted both the PDGFRA insulator site and CDKN2A in the brains of mice. A week later, they examined the brains and found an abnormally large number of cells within. In combination with a mitogen that induced cell division, these mice developed malignant gliomas with OPC markers, indicating that OPCs were the cells of origin for these tumors.
This is one of the first studies to show the direct effects of specific epigenetic changes in progenitor cells that become cancerous in vivo. Additionally, the confirmation that OPCs give rise to glioma could help researchers make targeted treatments. "This is a very interesting study that advances our understanding of how DNA hypermethylation contributes to cancer initiation,” said Katherine Chiapinelli, a professor at George Washington University who not involved in the study. A recent phase 3 clinical trial showed that Vorasidinib, a drug that inhibits mutant IDH1 and IDH2, significantly extended progression free survival in patients.5 “In the future it would be interesting to see whether patients who respond to these inhibitors exhibit loss of methylation at the regions identified," Chiapinelli said.
References
1. DeVita VT, Jr., Rosenberg SA. Two hundred years of cancer research. N Engl J Med. 2012;366(23):2207-2214.
2. Baylin SB, Jones PA. A decade of exploring the cancer epigenome - biological and translational implications. Nat Rev Cancer. 2011;11(10):726-734.
3. Rahme GJ, et al. Modeling epigenetic lesions that cause gliomas. Cell. 2023;186(17):3674-3685 e3614.
4. Flavahan WA, et al. Insulator dysfunction and oncogene activation in IDH mutant gliomas. Nature. 2016;529(7584):110-114.
5. Mellinghoff IK, et al. Vorasidenib in IDH1- or IDH2-mutant low-grade glioma. N Engl J Med. 2023;389(7):589-601.